NIAAA Director's Report on Institute Activities to the 147th Meeting of the National Advisory Council on Alcohol Abuse and Alcoholism
Table of Contents
- NIAAA BUDGET
- COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
- DIRECTOR'S ACTIVITIES
- STAFF TRANSITIONS
- HONORS & AWARDS
- NEW REQUESTS FOR APPLICATIONS AND PROGRAM ANNOUNCEMENTS
- NOTABLE NIAAA STAFF ACTIVITIES
- WHAT'S AHEAD
- NIH RESEARCH HIGHLIGHTS
- NIAAA COMMUNICATIONS ACTIVITIES
Fiscal Year (FY) 2017
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) closed FY 2017 on September 30, 2017; the final appropriation for NIAAA was $483.4 million. A summary of key funding actions within this appropriation follows:
- NIAAA awarded 649 research project grants (RPGs), including 201 competing awards, which translates to a success rate of 21.9 percent.
- NIAAA funded 20 research centers for $30.2 million.
- NIAAA funded 160 other research grants for $41.5 million, including career awards, one Cooperative Clinical Agreement, and several resource and conference grant awards.
- NIAAA supported 280 full-time training positions for $13.8 million.
- NIAAA funding for our Research and Development (R&D) contract portfolio was $38.6 million.
- NIAAA support for intramural research totaled $51 million.
FY 2018
The NIAAA is currently operating under H.R. 195, a Continuing Resolution (CR) until February 8, 2018. Following the National Institutes of Health (NIH) policy under the CR, all grants will be funded at 90 percent. This is consistent with NIH practice during the CRs of FY 2006–2017. Upward adjustments to awarded levels will be considered after FY 2018 appropriations are enacted, but NIH expects institutions to monitor their expenditures carefully during this period. All legislative mandates that were in effect in FY 2017 remain in effect under the CR.
Please note: Because NIAAA is operating under a CR, the budget mechanism table is not available at this time
FY 2019
Preliminary work on the budget for FY 2019 is beginning. After intermediate stages of review, the President’s budget request will be presented to Congress in February 2018, at which time it will become available to the public.
COLLABORATIVE RESEARCH ON ADDICTION AT NIH UPDATE
Adolescent Brain and Cognitive Development (ABCD) Study
The ABCD Study (https://www.abcdstudy.org/) continues to meet enrollment targets and currently has more than 7,300 nine- and ten-year old children enrolled. At this pace, enrollment will reach 11,400 by the end of the recruiting period. In June 2017, the study announced it has partnered with the National Institute of Mental Health (NIMH) Data Archive (NDA) to share ABCD Study data with the public on an ongoing basis. Currently, ABCD investigators are working with NDA to finalize the imaging and neuropsychological data from 4,500 subjects, which will be included in the first data release. Curated data, including all assessment domains and computational analysis pipelines, will be released annually through NDA. The first release is anticipated in February 2018.
The annual meeting of the ABCD investigators took place on November 8, 2017, and included a separate meeting of the Observational Safety and Monitoring Board. Updates from study sites and working groups indicate that the study is progressing very well. A concern about whether recruitment was meeting sociodemographic goals (i.e., achieving a balanced sample with regard to race, income, and parental education) was discussed at length. The December 2017 recruitment analysis is showing an improvement in meeting these goals (96 percent on target), but the issue continues to be monitored. At the November 8, 2017, meeting, progress was made on the development of a fair and efficient publication process to get ABCD study findings into the literature.
The CRAN Committee is continuing to work to develop a notice of funding opportunity that will encourage applications that use ABCD data to answer a variety of questions about alcohol, drug, and nicotine use and misuse, risk and protective factors, and effects on the developing brain.
NIAAA’s Director, George F. Koob, Ph.D., made several important presentations from August 2017 through December 2017.
- He was a keynote speaker at the Gordon Research Conference, Cannabinoid Function in the Central Nervous System Seminar in Waterville Valley, New Hampshire, on August 19, 2017. His talk was titled “Neurobiology of Addiction: A Negative Reinforcement Perspective.”
- He made a presentation to the California Society on Addiction Medicine in San Francisco, California, on August 26, 2017. His presentation was titled “The Neurobiology of Addiction.”
- He presented a featured talk titled, “Addiction Medicine: The Urgent Need for Trained Physicians,” at a congressional briefing sponsored by the Addiction Medicine Foundation and co-sponsored by the Congressional Prescription Drug Abuse Caucus, the Congressional Addiction, Treatment, and Recovery Caucus, and the Congressional Bipartisan Heroin Task Force on September 26, 2017.
- He presented at Columbia University Grand Rounds in New York, New York, on September 27, 2017. His presentation was titled “Alcohol and Drug Addiction: The Gain in the Brain is the Pain.”
- He spoke at Stellenbosch University in South Africa on September 27, 2017. His talk was titled “What Science Can Tell You about the Diagnosis, Prevention and Treatment of Alcoholism.”
- He spoke at the 2017 National Conference on Alcohol and Opioid Use Among Women and Girls in Washington, D.C., on October 27, 2017. His talk was titled “Alcohol and the Female Brain.”
- He spoke at the Neurobiology of Compulsive Behaviors: Translational Tools in Addiction meeting in Patterson, New Jersey, on November 8, 2017. His talk was titled “Neurobiology of Addiction: A Negative Reinforcement View.”
- He spoke at the Alcoholic Hepatitis: Pathogenesis, Treatment and Challenge meeting at The Johns Hopkins University in Baltimore, Maryland, on December 15, 2017. His talk was titled “Alcohol Addiction and Treatment.”
- He attended the Children’s Inn’s Congressional Reception in Washington, D.C., on January 17, 2018, along with NIH Director Dr. Francis S. Collins and Directors of other ICs.

STAFF TRANSITIONS
Departing Staff

Robert Huebner, Ph.D., who served as Acting Director of the Division of Treatment and Recovery Research (DTRR) at NIAAA, retired at the end of the 2017, after 31 years of federal service. Dr. Huebner was recruited to move to Washington, D.C., in 1986 to lead a project on homelessness commissioned by the Senate Labor and Human Resources Committee. He joined NIAAA in 1988 to oversee a national evaluation of the Institute’s research demonstration programs for the homeless. Later, he was appointed Chief of the newly created Health Services Research Branch, where he established the Institute’s health services research portfolio and oversaw the NIAAA National Advisory Council’s national plan for health services research. In 1999, he was appointed Deputy Director of the then Division of Clinical and Prevention Research and, four years later, appointed Deputy Director of the newly created DTRR. Dr. Huebner played a major role in the growth of NIAAA’s research portfolio on behavioral treatments and health services research and was actively involved in the Institute’s efforts to promote evidence-based therapies for alcohol use disorder (AUD) in everyday practice settings. In addition, he has been the recipient of numerous awards, including the Research Society on Alcoholism’s Seixas Award for Distinguished Service; the American Psychological Association’s Meritorious Research Service Award and Presidential Citation for Distinguished Service, and NIAAA’s Martin K. Trusty Excellence in Management Award. Dr. Huebner has numerous publications on alcohol treatment and served as co-editor of a special issue of Alcoholism: Clinical and Experimental Research titled “The Search for Mechanisms of Behavior Change in Evidence-Based Behavioral Treatments for Alcohol Use Disorders.” Most recently, Dr. Huebner oversaw the development and implementation of NIAAA’s Alcohol Treatment Navigator.

Tony Jourdan, Ph.D., a Research Fellow in NIAAA’s Laboratory of Physiological Studies left NIAAA to join the Lipid Research Group at University of Burgundy in Dijon, France, in a tenure-track faculty position from the Institut National de la Santé et de la Recherche Médicale (Inserm).
Ming-Jiang Xu, M.D., Ph.D., a Research Fellow in NIAAA’s Laboratory of Liver Disease was recruited by Novo Nordisk as a Research Scientist in their newly established Research Center in Beijing, China.
At the fourth annual NIAAA awards ceremony, NIAAA staff were recognized with the following awards:
- Daniel W. Hommer Memorial Award for Outstanding Fellow – Dr. Sofia Bouhlal
- Benedict J. Latteri Memorial Award for Excellence in Scientific Publication – Drs. Matthew Sloan and Joshua Gowin
- Advancing Diversity Award – Dr. Judith Arroyo
- Program Officer of the Year Award – Drs. Svetlana Radaeva and Mariela Shirley
- Scientific Achievement Award – Dr. Lorenzo Leggio
- Clinical Service Award – Dr. Mary Lee
- Support Award – Christie Halcomb
- Operational Excellence Award – Drs. Lori Ducharme and Robert Huebner, Maureen Gardner, and Gregory Roa
- Mentoring Award – Dr. Resat Cinar
- NIAAA Ambassador Award – Lynn Morin
- Martin K. Trusty Excellence in Management Award – Dr. George Kunos
Dr. George Kunos was recipient of an Honorary Doctorate from Semmelweis University in Budapest, Hungary.
Drs. George Kunos and Pal Pacher have been included in the list of Highly Cited Researchers 2017 in the Pharmacology and Toxicology field.
Dr. Kenner Rice has been elected to the rank of Fellow of the American Academy of Inventors.
NEW REQUESTS FOR APPLICATIONS (RFAs) AND PROGRAM ANNOUNCEMENTS (PAs)
Notice of Funding Opportunities (NOFO) Issued by NIAAA
Interaction of HIV Infection and Alcohol Abuse on Central Nervous System Morbidity Limited Competition (U01 Clinical Trial Not Allowed) RFA-AA-18-008. The purpose of this NOFO is to solicit applications that evaluate the cumulative and progressive effects on brain structure and cognitive/behavioral function of combined HIV infection and alcohol abuse.
Medications Development for the Treatment of Alcohol Use Disorder (U01 Clinical Trial Optional) RFA-AA-18-009. The purpose of this NOFO is to solicit cooperative agreement applications for research that advances promising compounds thorough the drug development pipeline for the treatment of AUD.
Investigational New Drug (IND)-Enabling Development of Medications to Treat Alcohol Use Disorder and Alcohol-Related Disorders (UT2 -Clinical Trial Optional) PAR-18-580; (U44 Clinical Trial Optional) PAR-18-578. This NOFO supports IND-enabling studies for the therapeutic candidate. Specifically, NIAAA will consider Small Business Innovation Research (SBIR) applications from small business concerns (SBCs) that propose the development of therapeutic agents for disorders that fall under the mission of NIAAA. An identified candidate, having sufficient bioactivity, stability, manufacturability, bioavailability, in vivo efficacy and/or target engagement, and other favorable properties that are consistent with the desired clinical application, is required prior to application.
Research on Comparative Effectiveness and Implementation of HIV/AIDS and Alcohol Interventions (R01 Clinical Trials Optional) PAS-18-557. This NOFO solicits applications that inform clinical decision-making to implement effective interventions that will improve prevention, care, and outcomes across the continuum of HIV and alcohol problem severity and patterns of alcohol use.
Effects of In Utero Alcohol Exposure on Adult Health and Disease (R01 Clinical Trial Optional) PA-18-507; (R21 Clinical Trial Optional) PA-18-508. This NOFO supports novel research on how prenatal alcohol exposure may contribute to the etiology of chronic diseases and health conditions later in life.
Wearable Alcohol Biosensors (R43/R44 Clinical Trial Optional) PAR-18-204. This NOFO solicits SBIR applications from eligible SBCs proposing to design and produce a non-invasive, discreet, wearable device to monitor blood alcohol levels in real time. Of particular interest are methods that quantify alcohol in blood or interstitial fluid as opposed to detection of alcohol that has exuded through the skin.
Epidemiology and Prevention in Alcohol Research (R01 Clinical Trial Optional) PA-18-390; (R21 - Clinical Trial Optional) PA-18-391. (R03 Clinical Trial Optional) PA-18-413. This NOFO solicits applications that focus on the epidemiology of alcohol use, alcohol-related harms, and AUD and the prevention of underage drinking, alcohol-related harms, and AUD.
Leveraging Electronic Health Records for Alcohol Services Research (R21/R33 Clinical Trial Optional) PAR-18-203. This NOFO seeks low-cost, pragmatic research projects that leverage electronic clinical records to conduct studies that address novel health services questions about the treatment of AUD in routine clinical care settings.
Human Studies to Evaluate Promising Medications to Treat Alcohol Use Disorder (R03 Clinical Trial Optional) PA-18-192; (R03 Clinical Trial Required) PA-18-198; (R21 Clinical Trial Required) PA-18-197. This NOFO supports applications that use human laboratory paradigms and/or clinical trials to evaluate the safety and efficacy of novel or re-purposed compounds, that bind to new targets, for treatment of AUD or AUD with a comorbid post-traumatic stress disorder.
Alcohol Use Disorders: Behavioral Treatment, Services and Recovery Research (R01 Clinical Trial Optional) PA-18-194; (R03 Clinical Trial Optional) PA-18-201; (R21 Clinical Trial Optional) PA-18-202. This NOFO supports grant applications that propose to support research on behavioral treatment for AUD; organizational, financial, and management factors that facilitate or inhibit the delivery of services for AUD; and phenomenon of recovery from AUD.
Screening and Brief Alcohol Interventions in Underage and Young Adult Populations (R01 Clinical Trial Optional) PA-18-193; (R03 Clinical Trial Optional) PA-18-200; (R21 Clinical Trial Optional) PA-18-199. This NOFO supports research on screening and brief interventions to prevent and/or reduce alcohol use and alcohol-related harms among underage and young adult populations.
Increasing the Use of Medications for the Treatment of Alcohol Use Disorders (R01 Clinical Trial Optional) PAR-18-196; This NOFO supports health services research designed to increase the public health impact of U.S. Food and Drug Administration (FDA)-approved pharmacotherapies for the treatment of AUD.
Program for Extramural/Intramural Alcohol Research Collaborations (U01 Clinical Trial Optional) PAR-18-195. This NOFO solicits applications to encourage collaboration between alcohol researchers in the extramural community and those within the NIAAA intramural research program.
Alcohol Impairment of Immune Function, Host Defense and Tissue Homeostasis (R01 Clinical Trial Optional) PA-18-191. This NOFO supports applications from researchers with broad expertise to study the consequences of alcohol consumption on immune function with a goal toward improving the outcome of patients who abuse alcohol.
NIH-Wide NOFOs with NIAAA’s Participation
Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiatives:
- Next-Generation Invasive Devices for Recording and Modulation in the Human Central Nervous System (UG3/UH3 - Clinical Trial Required) RFA-NS-18-021; (U44 Clinical Trial Required) RFA-NS-18-022
- Clinical Studies to Advance Next-Generation Invasive Devices for Recording and Modulation in the Human Central Nervous System (UH3 Clinical Trial Required) RFA-NS-18-023
- Development, Optimization, and Validation of Novel Tools and Technologies for Neuroscience Research (Small Business Technology Transfer) (R41/R42 Clinical Trial Not Allowed) PAR-18-515; (SBIR) (R43/R44 Clinical Trial Not Allowed) PAR-18-501
- Targeted BRAIN Circuits Planning Projects - TargetedBCPP (R34 Clinical Trials Not Allowed) RFA-NS-18-014
- Biology and Biophysics of Neural Stimulation (R01 Clinical Trials Optional) RFA-NS-18-018
- Ruth L. Kirschstein National Research Service Award (NRSA) Individual Postdoctoral Fellowship (F32) RFA-MH-18-510
- Tools to Target, Identify and Characterize Non-Neuronal Cells in the Brain (R01 Clinical Trial Not Allowed) RFA-DA-18-018
- Development of Next Generation Human Brain Imaging Tools and Technologies (U01) (Clinical Trials Not Allowed) RFA-EB-17-004
- Proof of Concept Development of Early Stage Next Generation Human Brain Imaging (R01 Clinical Trials Not Allowed) RFA-EB-17-003
- Theories, Models and Methods for Analysis of Complex Data from the Brain (R01 Clinical Trial Not Allowed) RFA-EB-17-005
Integrative Research on Polysubstance Abuse and Addiction (R21/R33 Clinical Trial Optional) PAR-18-084
Testing Interventions for Health-Enhancing Physical Activity (R01 Clinical Trial Optional) PAR-18-324
Simulation Modeling and Systems Science to Address Health Disparities (R01 Clinical Trial Not Allowed) PAR-18-331
Accelerating the Pace of Drug Abuse Research Using Existing Data (R01 Clinical Trial Optional) PAR-18-062
Addressing Health Disparities through Effective Interventions Among Immigrant Populations (R01 Clinical Trial Optional) PA-18-284; (R21 Clinical Trial Optional) PA-18-285
Health Services and Economic Research on the Prevention and Treatment of Drug, Alcohol, and Tobacco Abuse (R01, Clinical Trial Optional) PA-18-569; (UG3/UH3 Clinical Trial Optional)
Blueprint Neurotherapeutics Network (BPN): Small Molecule Drug Discovery and Development for Disorders of the Nervous System (U44) - Clinical Trial Optional PAR-18-541; (UG3/UH3 Clinical Trial Optional) PAR-18-546
Innovation Corps (I-Corps) at NIH Program for NIH and [U.S. Centers for Disease Control and Prevention] Translational Research (Admin Supp - Clinical Trial Not Allowed) PA-18-517
Developing the Therapeutic Potential of the Endocannabinoid System for Pain Treatment (R01 Clinical Trial Optional) PA-18-465
Multi-Site Pilot and Feasibility Studies for System-Level Implementation of Substance Use Prevention and Treatment Services (R34 Clinical Trial Optional) PAR-18-223 (R01 Clinical Trial Optional) PAR-18-222
Health Services Research on Minority Health and Health Disparities (R01 Clinical Trial Optional) PAR-18-286; (R21 Clinical Trial Optional) PAR-18-287
Multidisciplinary Studies of HIV/AIDS and Aging (R21 Clinical Trial Optional) PAR-18-190
Methodology and Measurement in the Behavioral and Social Sciences (R01 Clinical Trials Optional) PAR-18-352; (R21 Clinical Trials Optional) PAR-18-378
National Cooperative Drug/Device Discovery/Development Groups (NCDDG) for the Treatment of Mental or Substance Use Disorders or Alcohol Addiction (U19 Clinical Trial Optional) PAR-18-230
Target Assessment, Engagement and Data Replicability to Improve Substance Use Disorders Treatment Outcomes (R21/R33 Clinical Trial Optional) PAR-18-086; (R33 Clinical Trial Optional) PAR-18-085
Health Services and Economic Research on the Prevention and Treatment of Drug, Alcohol, and Tobacco Abuse (R03 Clinical Trial Optional) PA-18-069; (R21 Clinical Trial Optional) PA-18-070
Pilot Health Services and Economic Research on the Treatment of Drug, Alcohol, and Tobacco Abuse (R34 Clinical Trial Optional) PA-18-068
Pilot and Feasibility Studies in Preparation for Drug and Alcohol Abuse Prevention Trials (R34 Clinical Trial Optional) PA-18-067
Bioengineering Research Partnerships (U01 Clinical Trial Optional) PAR-18-208
NIH Blue Print: Development and Validation of Technologies for Rapid Isolation and Characterization of Extracellular Vesicles of Central Nervous System Origin (R21/R33 Clinical Trial Not Allowed) RFA-MH-18-600
The Health of Sexual and Gender Minority (SGM) Populations (R01 Clinical Trial Optional) PA-18-037
Dissemination and Implementation Research in Health (R21 Clinical Trial Optional) PAR-18-017; (R01 Clinical Trial Optional) PAR-18-007
Diet and Physical Activity Assessment Methodology (R21 Clinical Trial Optional) PAR-18-112; (R01 Clinical Trial Optional) PA-18-010
Behavioral and Integrative Treatment Development Program (R03 Clinical Trial Optional) PA-18-074; (R34 Clinical Trial Optional) PA-18-073; (R01 Clinical Trial Optional) PA-18-055
Research to Improve Native American Health (R21 Clinical Trial Optional) PAR-17-464
Intervention Research to Improve Native American Health (R01 Clinical Trial Optional) PAR-17-496
Addressing Health Disparities through Effective Interventions Among Immigrant Populations (R21 Clinical Trial Optional) PA-18-285; (R01 Clinical Trial Optional) PA-18-284
Simulation Modeling and Systems Science to Address Health Disparities (R01 Clinical Trial Not Allowed) PAR-18-331
Testing Interventions for Health-Enhancing Physical Activity (R01 Clinical Trial Optional) PAR-18-324
NOTABLE NIAAA STAFF ACTIVITIES -- AUGUST 2017 - DECEMBER 2017
Drs. George F. Koob and Lori Ducharme presented an overview of the NIAAA Alcohol Treatment NavigatorSM: Pointing the Way to Evidence Based Care at a congressional briefing on October 30, 2017. The briefing was sponsored by the Friends of NIAAA and the Addiction, Treatment and Recovery Caucus.


Dr. Lori Ducharme was an invited speaker for several events and activities to promote the launch of the NIAAA Alcohol Treatment Navigator. These included a national webinar; radio appearances (KOMO Radio – Seattle and SiriusXM’s Doctor Radio); interviews with the Associated Press and Alcohol & Drug Abuse Weekly; a Twitter chat (co-hosted with the American Society of Addiction Medicine (ASAM)); a Facebook Live event (hosted by the Addiction Policy Forum); and blog posts (for the Recovery Research Institute and Substance Abuse and Mental Health Services Administration’s Addiction Technology Transfer Center network). She also made five presentations to the annual meeting of the American Association for the Study of Liver Diseases (AASLD) on October 22 and 23, 2017, to introduce the Navigator. Her schedule included four talks at the Tech Bar of the AASLD meeting, open to an audience of clinician hepatologists, basic researchers, and meeting attendees, as well as a meet-and-greet session in the Associates Lounge, a setting with a focus for registered nurses, nurse practitioners, physician assistants, pharmacists, and other mid-level hepatology providers.
Dr. M. Katherine Jung chaired a session on “Pathogenesis and Treatment of Alcoholic Hepatitis” at the NIAAA-Johns Hopkins Joint Symposium on Alcoholic Hepatitis on December 15, 2017, in Baltimore, Maryland.
Dr. Lorenzo Leggio was invited to join the Scientific Committee of the Zardi-Gori Foundation (Milan, Italy), a non-profit organization focused on promoting research and education on addictions. The Foundation recently organized a 2-day scientific meeting titled “Alcohol Use Disorder: from Bench to Bedside” for which Dr. Leggio served on the Scientific Committee. Drs. Lorenzo Leggio, David Goldman, and George Kunos made presentations and chaired symposia at the meeting which took place on November 20 and 21, 2017, in Milan, Italy.
Drs. Changhai Cui, George F. Koob, John Matochik, Antonio Noronha and Soundar Regunathan presented and chaired sessions at the mini-convention on “Frontiers in Addiction Research: The Sciences of Astrocytes, Stress Response, and Translational Research” sponsored by the National Institute on Drug Abuse (NIDA) and NIAAA in conjunction with the Annual Meeting of the Society for Neuroscience, on November 10, 2017, in Washington, D.C. Three scientific sessions of the mini-convention explored: 1) techniques and approaches for studying astrocytes in neurological disorders and behavior; 2) stress reactivity and immune function in brain development, addiction, and depression; and 3) approaches towards treatment of substance abuse disorders and mental illness.
Dr. Deidra Roach, M.D., co-chaired, with a colleague from NIDA, the first National Conference on Alcohol and Opioid Use in Women and Girls, at which Dr. George F. Koob gave a keynote address (see Director’s Activities), held October 26 and 27, 2017, in Washington, D.C.
Dr. Abbas Parsian, organized a symposium for the 2017 World Congress of Psychiatric Genetics Scientific Meeting that was held October 13–17, 2017, in Orlando, Florida. The symposium titled, “Genetics of addiction: New findings from sequencing studies and beyond” focused on the results of whole-exome sequencing projects and how the functional variations could be studied in stem cells and animal models.
Dr. Raye Litten presented “Advances and Research Strategies to Treat Alcohol Use Disorder in Veterans” as part of the ASAM Veteran Webinar in Rockville, Maryland, on October 5, 2017.
Dr. Lorenzo Leggio was a Keynote Speaker at the Italian Association for Liver Studies Meeting, “Alcoholic Liver Disease: The New Challenge” in Rome, Italy, on October 5, 2017.
Gregory Bloss co-organized a symposium titled “Turning Discovery into Health: The Contributions of Economic Research” held September 28 and 29, 2017 on the NIH campus and sponsored by the NIH Common Fund Health Economics Program.
Dr. Mariela Shirley served as a panel member for the Military Operational Medicine Research Program/Joint Program Committee for Military Operational Medicine Substance Abuse Research In-Progress Review of Defense Health Program-funded research on September 27 and 28, 2017, in Frederick, Maryland.
Dr. Robert Freeman organized a workshop, “NIAAA Workshop to Explore Research Needs in Addressing Alcohol-Related Suicide,” held on September 19 and 20, 2017, at NIAAA in Rockville, Maryland. The meeting, co-funded by the NIH Office of Disease Prevention, featured talks on the epidemiology, etiology, prevention and treatment of alcohol-related suicide. Speakers included NIAAA’s Drs. Aaron White, Rosalind Breslow, Raye Litten, Ralph Hingson and Michael Hilton, as well as NIAAA grantees.
Drs. Margaret (Peggy) Murray and Kenneth Warren were invited plenary speakers at a joint meeting of the Japanese Society for Alcohol-Related Problems and the Japanese Medical Society of Alcohol and Addiction Studies, Yokohama, Japan, on September 7 and 8, 2017. Dr. Murray’s talk was titled “Screening and Brief Intervention: Where it Works, Where it Might Work, Where it Does Not Work, and What We Need from Research.” Dr. Warren spoke on the history of fetal alcohol spectrum disorders. Dr. Warren also made a special presentation to senior staff of the two societies on the organization of NIAAA, the NIAAA research portfolio, and how research grants at the NIH are reviewed and funded.
Dr. Peggy Murray was an invited member of an expert panel to discuss the development of future directions for research on Screening and Brief Intervention held in conjunction with the International Network on Brief Interventions for Alcohol & Other Drugs on September 1, 2017, at New York University School of Medicine in New York, New York.
Dr. Veronica Alvarez was an invited speaker at the Gordon Research Conference in Catecholamines that was held August 13–17, 2017, in Newry, Maine, where she presented a talk titled “Opposing Effects of Drugs of Abuse on Dopamine Transmission in the Striatum.”
The FDA has issued an IND for JD-5037, the first in-class peripheral CB1 receptor antagonist for the treatment of non-alcoholic steatohepatitis. The IND was based on preclinical studies by Dr. George Kunos’s laboratory and on IND-enabling studies supported by a Bridging Interventional Development Gaps grant from the National Center for Advancing Translational Sciences. Phase I studies are expected to begin in 2018.
The 2018 Gordon Research Conference (GRC) on Alcohol and the Nervous System will be held March 4–9, 2018, Galveston, Texas. The conference will cover a broad range of studies at the molecular, cellular, circuit/systems and behavioral levels, emphasizing multidisciplinary work and innovative approaches. This GRC will be held in conjunction with the Gordon Research Seminar on Alcohol and the Nervous System on March 3 and 4, 2018, in Galveston, Texas.
The Fourth Annual BRAIN Initiative Investigators Meeting will be held April 9–11, 2018, at the Bethesda North Marriott Hotel and Conference Center, Bethesda, Maryland. The purpose of this meeting is to provide a forum to discuss developments supported by the BRAIN initiative and potential new directions, and to identify areas for collaboration and research coordination. It will convene BRAIN Initiative awardees, staff, and leadership from the contributing federal agencies.
Significance: Activation of innate immunity is a critical component in the development of alcoholic liver disease (ALD). Previous studies suggest that the 35 kD size hyaluronic acid (HA35), which has potential anti-inflammatory effects and the ability to protect the integrity of the intestinal barrier, could have protective effects on the liver in the face of ethanol exposure. This study evaluated the effect of HA35 on ethanol-induced sensitization of Kupffer cells (specialized macrophages located in the liver) and ethanol-induced liver injury in mice. Results showed that HA35 had an anti-inflammatory effect on Kupffer cells following ethanol treatment and that a specific micro RNA (miRNA), miR181b-3p, is dynamically regulated by HA35 and ethanol. These findings identify two potential new targets, HA35 and miR181b-3p, that may have therapeutic potential for the treatment of alcoholic liver disease.
Increased inflammatory signaling by Kupffer cells contributes to alcoholic liver disease (ALD). Here we investigated the impact of small, specific-sized hyaluronic acid of 35 kD (HA35) on ethanol-induced sensitization of Kupffer cells, as well as ethanol-induced liver injury in mice. Unbiased analysis of microRNA (miRNA) expression in Kupffer cells identified miRNAs regulated by both ethanol and HA35. Toll-like receptor 4 (TLR4)-mediated signaling was assessed in primary cultures of Kupffer cells from ethanol- and pair-fed rats after treatment with HA35. Female C57BL6/J mice were fed ethanol or pair-fed control diets and treated or not with HA35. TLR4 signaling was increased in Kupffer cells by ethanol; this sensitization was normalized by ex vivo treatment with HA35. Next generation sequencing of Kupffer cell miRNA identified miRNA 181b-3p (miR181b-3p) as sensitive to both ethanol and HA35. Importin α5, a protein involved in p65 translocation to the nucleus, was identified as a target of miR181b-3p; importin α5 protein was increased in Kupffer cells from ethanol-fed rats, but decreased by HA35 treatment. Overexpression of miR181b-3p decreased importin α5 expression and normalized lipopolysaccharide-stimulated tumor necrosis factor α expression in Kupffer cells from ethanol-fed rats. In a mouse model of ALD, ethanol feeding decreased miR181b-3p in liver and increased expression of importin α5 in nonparenchymal cells. Treatment with HA35 normalized these changes and also protected mice from ethanol-induced liver and intestinal injury. CONCLUSION: miR181b-3p is dynamically regulated in Kupffer cells and mouse liver in response to ethanol and treatment with HA35. miR181b-3p modulates expression of importin α5 and sensitivity of TLR4-mediated signaling. This study identifies a miR181b-3p-importin α5 axis in regulating inflammatory signaling pathways in hepatic macrophages. (Saikia P, Bellos D, McMullen MR, Pollard KA, de la Motte C, and Nagy LE. Hepatology. 2017 Aug; 66(2):602-615. doi: 10.1002/hep.29144. Epub 2017 Jul 4)
Significance: Micro RNA122 (miR122), the most abundant liver miRNA, has been implicated in the regulation of fatty acid and cholesterol metabolism. This study observed a reduction of miR122 in the livers of patients with alcoholic liver disease as well as in alcohol-fed mice. Increasing miR122 expression therapeutically in mice mitigated alcohol-induced liver injury and fibrosis, whereas injecting anti-miR122 increased steatosis, inflammation, and serum levels of alanine aminotransferase, highlighting that alcohol-induced changes to the miR122 pathway play a role in developing alcoholic liver disease. Lastly, the study identified transcription factor GRHL2 (grainyhead-like 2) as an upstream regulator, and HIF1A (hypoxia-inducible factor 1A) as a downstream effector of miR122.
BACKGROUND & AIMS: Chronic, excessive alcohol consumption leads to alcoholic liver disease (ALD) characterized by steatosis, inflammation, and eventually cirrhosis. The hepatocyte specific microRNA 122 (MIR122) regulates hepatocyte differentiation and metabolism. We investigated whether an alcohol-induced decrease in level of MIR122 contributes to development of ALD.
METHODS: We obtained liver samples from 12 patients with ALD and cirrhosis and 9 healthy individuals (controls) and analyzed them by histology and immunohistochemistry. C57Bl/6 mice were placed on a Lieber-DeCarli liquid diet, in which they were fed ethanol for 8 weeks, as a model of ALD, or a control diet. These mice were also given injections of CCl4, to increase liver fibrosis, for 8 weeks. On day 28, mice with ethanol-induced liver disease and advanced fibrosis, and controls, were given injections of recombinant adeno-associated virus 8 vector that expressed the primary miR-122 transcript (pri-MIR122, to overexpress MIR122 in hepatocytes) or vector (control). Two weeks before ethanol feeding, some mice were given injections of a vector that expressed an anti-MIR122, to knock down its expression. Serum and liver tissues were collected; hepatocytes and liver mononuclear cells were analyzed by histology, immunoblots, and confocal microscopy. We performed in silico analyses to identify targets of MIR122 and chromatin immunoprecipitation quantitative PCR analyses in Huh-7 cells. RESULTS: Levels of MIR122 were decreased in liver samples from patients with ALD and mice on the Lieber-DeCarli diet, compared with controls. Transgenic expression of MIR122 in hepatocytes of mice with ethanol-induced liver disease and advanced fibrosis significantly reduced serum levels of alanine aminotransferase (ALT) and liver steatosis and fibrosis, compared to mice given injections of the control vector. Ethanol feeding reduced expression of pri-MIR122 by increasing expression of the spliced form of the transcription factor grainyhead like transcription factor 2 (GRHL2) in livers tissues from mice. Levels of GRHL2 were also increased in liver tissues from patients with ALD, compared with controls; increases correlated with decreases in levels of MIR122 in human liver. Mice given injections of the anti-MIR122 before ethanol feeding had increased steatosis, inflammation, and serum levels of ALT compared to mice given a control vector. Levels of hypoxia inducible factor 1 alpha (HIF1A) mRNA, a target of MIR122, were increased in liver tissues from patients and mice with ALD, compared with controls. Mice with hepatocyte-specific disruption of Hif1a developed less-severe liver injury following administration of ethanol, injection of anti-MIR122, or both. CONCLUSIONS: Levels of MIR122 decrease in livers from patients with ALD and mice with ethanol-induced liver disease, compared with controls. Transcription of MIR122 is inhibited by GRHL2, which is increased in livers of mice and patients with ALD. Expression of an anti-MIR122 worsened the severity of liver damage following ethanol feeding in mice. MIR122 appears to protect the liver from ethanol-induced damage by reducing levels of HIF1A. These processes might be manipulated to reduce the severity of ALD in patients. (Satishchandran A, Ambade A, Rao S, Hsueh YC, Iracheta-Vellve A, Tornai D, Lowe P, Gyongyosi B, Li J, Catalano D, Zhong L, Kodys K, Xie J, Bala S, Gao G and Szabo G. Gastroenterology. 2018 Jan; 154(1):238-252.e7. doi: 10.1053/j.gastro.2017.09.022. Epub 2017 Oct 4)
Significance: Cannabidiol (CBD) is a non-psychoactive constituent of marijuana, which has anti-inflammatory effects. This study investigated the effects of CBD on liver injury induced by chronic plus binge alcohol feeding in mice. The findings demonstrate that CBD attenuates alcohol-induced liver injury by decreasing neutrophil-mediated oxidative injury, inflammation, and pathological metabolic reprograming. These observations suggest that CBD may emerge as a novel treatment for alcoholic liver disease.
Cannabidiol (CBD) is a non-psychoactive component of marijuana, which has anti-inflammatory effects. It has also been approved by FDA for various orphan diseases for exploratory trials. Herein, we investigated the effects of CBD on liver injury induced by chronic plus binge alcohol feeding in mice. CBD or vehicle was administered daily throughout the alcohol feeding study. At the conclusion of the feeding protocol, serums samples, livers or isolated neutrophils were utilized for molecular biology, biochemistry and pathology analysis. CBD significantly attenuated the alcohol feeding-induced serum transaminase elevations, hepatic inflammation (mRNA expressions of TNFα, MCP1, IL1β, MIP2 and E-Selectin, and neutrophil accumulation), oxidative/nitrative stress (lipid peroxidation, 3-nitrotyrosine formation, and expression of reactive oxygen species generating enzyme NOX2). CBD treatment also attenuated the respiratory burst of neutrophils isolated from chronic plus binge alcohol fed mice or from human blood, and decreased the alcohol-induced increased liver triglyceride and fat droplet accumulation. Furthermore, CBD improved alcohol-induced hepatic metabolic dysregulation and steatosis by restoring changes in hepatic mRNA or protein expression of ACC-1, FASN, PPARα, MCAD, ADIPOR-1, and mCPT-1. Thus, CBD may have therapeutic potential in the treatment of alcoholic liver diseases associated with inflammation, oxidative stress and steatosis, which deserves exploration in human trials. (Wang Y, Mukhopadhyay P, Cao Z, Wang H, Feng D, Haskó G, Mechoulam R, Gao B, and Pacher P. Sci Reps. 2017 Sep 21; 7(1):12064. doi: 10.1038/s41598-017-10924-8)
Phosphodiesterase 4b Expression Plays a Major Role in Alcohol-Induced Neuro-inflammation
Significance: Phosphodiesterase 4b (Pde4b) is known for its specific expression in brain tissue and immune cells, and has multiple functions, including regulating neurotransmission, metabolism, and sustaining a pro-inflammatory response. Numerous past studies have shown that Pde4b inhibitors, administrated in rodents, reduce alcohol abstinence-induced anxiety, depressive behavior, and consumption. Using a mouse model of chronic alcohol feeding, this study examined the causal role of Pde4b expression in alcohol-induced neuro-inflammation. The results demonstrate that alcohol feeding in mice increases Pde4b expression in the brain tissue. Furthermore, they establish a functional connection between the Pde4b expression and alcohol-induced increase of inflammatory mediators in the brain, as administration of a Pde4b inhibitor, rolipram, attenuates the increase of brain inflammatory markers in alcohol-fed wildtype mice. These data support future testing of FDA-approved phosphodiesterase inhibitors as potential interventions for alcohol-related systemic and neuropathological conditions.
It is increasingly evident that alcohol-induced, gut-mediated peripheral endotoxemia plays a significant role in glial cell activation and neuro-inflammation. Using a mouse model of chronic alcohol feeding, we examined the causal role of endotoxin- and cytokine-responsive Pde4 subfamily b (Pde4b) expression in alcohol-induced neuro-inflammation. Both pharmacologic and genetic approaches were used to determine the regulatory role of Pde4b. In C57Bl/6 wild type (WT) alcohol fed (WT-AF) animals, alcohol significantly induced peripheral endotoxemia and Pde4b expression in brain tissue, accompanied by a decrease in cAMP levels. Further, along with Pde4b, there was a robust activation of astrocytes and microglia accompanied by significant increases in the inflammatory cytokines (Tnfα, Il-1β, Mcp-1 and Il-17) and the generalized inflammatory marker Cox-2. At the cellular level, alcohol and inflammatory mediators, particularly LPS, Tnfα and Hmgb1 significantly activated microglial cells (Iba-1 expression) and selectively induced Pde4b expression with a minimal to no change in Pde4a and d isoforms. In comparison, the alcohol-induced decrease in brain cAMP levels was completely inhibited in WT mice treated with the Pde4 specific pharmacologic inhibitor rolipram and in Pde4b-/- mice. Moreover, all the observed markers of alcohol-induced brain inflammation were markedly attenuated. Importantly, glial cell activation induced by systemic endotoxemia (LPS administration) was also markedly decreased in Pde4b-/- mice. Taken together, these findings strongly support the notion that Pde4b plays a critical role in coordinating alcohol-induced, peripheral endotoxemia mediated neuro-inflammation and could serve as a significant therapeutic target. (Avila DV, Myers SA, Zhang J-W, Kharebava G, McClain CJ, Kim, H-Y, Whittemore SR, Gobejishvili L, and Barve S. Neuropharmacology. 2017 Oct; 125: 376-385. doi: 10.1016/j.neuropharm.2017.08.011. Epub 2017 Aug 12)
Parallel, but Dissociable, Processing in Discrete Corticostriatal Inputs Encodes Skill Learning
Significance: This study used fiber photometry to evaluate real-time activity of associative inputs from the medial prefrontal cortex to the dorsomedial striatum and sensorimotor inputs from motor cortex to dorsolateral striatum in mice. Findings showed co-engagement of associative and sensorimotor inputs early in action learning. Disengagement of associative, but not sensorimotor, inputs predicted individual differences in subsequent skill learning. Divergent somatic and presynaptic engagement in both projections during early action learning suggests potential learning-related in vivo modulation of presynaptic corticostriatal function.
Changes in cortical and striatal function underlie the transition from novel actions to refined motor skills. How discrete, anatomically defined corticostriatal projections function in vivo to encode skill learning remains unclear. Using novel fiber photometry approaches to assess real-time activity of associative inputs from medial prefrontal cortex to dorsomedial striatum and sensorimotor inputs from motor cortex to dorsolateral striatum, we show that associative and sensorimotor inputs co-engage early in action learning and disengage in a dissociable manner as actions are refined. Disengagement of associative, but not sensorimotor, inputs predicts individual differences in subsequent skill learning. Divergent somatic and presynaptic engagement in both projections during early action learning suggests potential learning-related in vivo modulation of presynaptic corticostriatal function. These findings reveal parallel processing within associative and sensorimotor circuits that challenges and refines existing views of corticostriatal function and expose neuronal projection- and compartment-specific activity dynamics that encode and predict action learning. (Kupferschmidt DA, Juczewski K, Cui G, Johnson KA, and Lovinger DM. Neuron. 2017 Oct 11; 96(2):476-489.e5. doi: 10.1016/j.neuron.2017.09.040)
Significance: This study used optogenetics to explore the role of cholinergic neurons in the nucleus accumbens (NAc) on dopamine transmission. Findings showed that CB1 agonists and endocannabinoids (eCBs) inhibited this increase in dopamine transmission, both in the NAc and the prefrontal cortex (PFC). These same CB1 receptors also modulate optical self-stimulation maintained by PFC afferent activation in the NAc.
Dopamine (DA) transmission mediates numerous aspects of behavior. Although DA release is strongly linked to firing of DA neurons, recent developments indicate the importance of presynaptic modulation at striatal dopaminergic terminals. The endocannabinoid (eCB) system regulates DA release and is a canonical gatekeeper of goal-directed behavior. Here we report that extracellular DA increases induced by selective optogenetic activation of cholinergic neurons in the nucleus accumbens (NAc) are inhibited by CB1 agonists and eCBs. This modulation requires CB1 receptors on cortical glutamatergic afferents. Dopamine increases driven by optogenetic activation of prefrontal cortex (PFC) terminals in the NAc are similarly modulated by activation of these CB1 receptors. We further demonstrate that this same population of CB1 receptors modulates optical self-stimulation sustained by activation of PFC afferents in the NAc. These results establish local eCB actions on PFC terminals within the NAc that inhibit mesolimbic DA release and constrain reward-driven behavior. (Mateo Y, Johnson KA, Covey DP, Atwood BK, Wang HL, Zhang S, Gildish I, Cachope R, Bellocchio L, Guzmán M, Morales M, Cheer JF, and Lovinger DM. Neuron. 2017 Dec 6; 96(5):1112-1126.e5. doi: 10.1016/j.neuron.2017.11.012)
Significance: This study provides mechanistic understanding of how early-life stress during adolescence contributes to alcohol addiction vulnerability. Using a rodent model of adolescent social isolation, Almonte et al. demonstrate that the chronic stress during adolescence impairs synaptic activities in the ventral hippocampus, a brain region that plays an integral role in mediating emotional behaviors. These neuroadaptations may contribute to addiction-vulnerable phenotype associated with early-life stress.
It has long been appreciated that adolescence represents a uniquely vulnerable period when chronic exposure to stressors can precipitate the onset of a broad spectrum of psychiatric disorders and addiction in adulthood. However, the neurobiological substrates and the full repertoire of adaptations within these substrates making adolescence a particularly susceptible developmental stage are not well understood. Prior work has demonstrated that a rodent model of adolescent social isolation (aSI) produces robust and persistent increases in phenotypes relevant to anxiety/stressor disorders and alcohol addiction, including anxiogenesis, deficits in fear extinction, and increased ethanol consumption. Here, we used extracellular field recordings in hippocampal slices to investigate adaptations in synaptic function and synaptic plasticity arising from aSI. We demonstrate that this early life stressor leads to enhanced excitatory synaptic transmission and decreased levels of long-term potentiation at hippocampal Schaffer collateral-CA1 synapses. Further, these changes were largely confined to the ventral hippocampus. As the ventral hippocampus is integral to neurocircuitry that mediates emotional behaviors, our results add to mounting evidence that aSI has profound effects on brain areas that regulate affective states. These studies also lend additional support to our recent proposal of the aSI model as a valid model of alcohol addiction vulnerability. (Almonte AG, Ewin SE, Mauterer MI, Morgan JW, Carter ES, and Weiner JL. Sci Rep. 2017 Sep 26;7(1):12300. doi: 10.1038/s41598-017-12531-z)
Methylomic Profiling and Replication Implicates Deregulation of PCSK9 in Alcohol Use Disorder
Significance: This study includes cross-tissue and cross-phenotypic analysis of genome-wide methylomic variation in individuals with alcohol use disorder (AUD), using samples from 3 discovery, 4 replication, and 2 translational cohorts. Results identified a differentially methylated region in the promoter of the proprotein convertase subtilisin/kexin 9 (PCSK9) gene that was associated with disease phenotypes. Biological validation showed that PCSK9 promoter methylation is conserved across tissues and positively correlated with expression. Mild alcohol use was associated with lower PCSK9 levels, while heavy chronic use resulted in increased PCSK9 levels. This finding links alcohol use to epigenetic changes in PCSK9, a key regulator in cholesterol homeostasis, possibly explaining the effects of alcohol on lipid metabolism and cardiovascular risk, with light alcohol use generally being protective while chronic heavy use having detrimental health outcomes.
Alcohol use disorder (AUD) is a common and chronic disorder with substantial effects on personal and public health. The underlying pathophysiology is poorly understood but strong evidence suggests significant roles of both genetic and epigenetic components. Given that alcohol affects many organ systems, we performed a cross-tissue and cross-phenotypic analysis of genome-wide methylomic variation in AUD using samples from 3 discovery, 4 replication, and 2 translational cohorts. We identified a differentially methylated region in the promoter of the proprotein convertase subtilisin/kexin 9 (PCSK9) gene that was associated with disease phenotypes. Biological validation showed that PCSK9 promoter methylation is conserved across tissues and positively correlated with expression. Replication in AUD datasets confirmed PCSK9 hypomethylation and a translational mouse model of AUD showed that alcohol exposure leads to PCSK9 downregulation. PCSK9 is primarily expressed in the liver and regulates low-density lipoprotein cholesterol (LDL-C). Our finding of alcohol-induced epigenetic regulation of PCSK9 represents one of the underlying mechanisms between the well-known effects of alcohol on lipid metabolism and cardiovascular risk, with light alcohol use generally being protective while chronic heavy use has detrimental health outcomes. (Lohoff FW, Sorcher JL, Rosen AD, Mauro KL, Fanelli RR, Momenan R, Hodgkinson CA, Vendruscolo LF, Koob GF, Schwandt M, George DT, Jones IS, Holmes A, Zhou Z, Xu MJ, Gao B, Sun H, Phillips MJ, Muench C, and Kaminsky ZA. Mol Psychiatry. 2017 Aug 29. doi:10.1038/mp.2017.168. Epub ahead of print)
Altered Brain Developmental Trajectories in Adolescents After Initiating Drinking
Significance: In a study from the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA), researchers looked for differences in adolescent brain growth associated with alcohol use. Three yearly magnetic resonance imaging (MRI) scans quantified cortical and white matter volumes. No-/low-alcohol-use adolescents were compared to moderate- or heavy-drinking adolescents. For no/low drinkers, gray matter volume declined throughout adolescence, while white matter regions grew faster at younger ages and slowed toward young adulthood. Heavy drinkers, but not moderate drinkers, diverged from no/low adolescents. Neither marijuana co-use nor baseline brain volumes contributed to the alcohol effect. These results provide evidence that initiation of heavy alcohol drinking during adolescence can disrupt normal changes in cortical gray matter regions.
The authors sought evidence for altered adolescent brain growth trajectory associated with moderate and heavy alcohol use in a large national, multisite, prospective study of adolescents before and after initiation of appreciable alcohol use. This study examined 483 adolescents (ages 12–21) before initiation of drinking and 1 and 2 years later. At the 2-year assessment, 356 participants continued to meet the study’s no/low alcohol consumption entry criteria, 65 had initiated moderate drinking, and 62 had initiated heavy drinking. MRI was used to quantify regional cortical and white matter volumes. Percent change per year (slopes) in adolescents who continued to meet no/low criteria served as developmental control trajectories against which to compare those who initiated moderate or heavy drinking. In no/low drinkers, gray matter volume declined throughout adolescence and slowed in many regions in later adolescence. Complementing gray matter declines, white matter regions grew at faster rates at younger ages and slowed toward young adulthood. Youths who initiated heavy drinking exhibited an accelerated frontal cortical gray matter trajectory, divergent from the norm. Although significant effects on trajectories were not observed in moderate drinkers, their intermediate position between no/low and heavy drinkers suggests a dose effect. Neither marijuana co-use nor baseline volumes contributed significantly to the alcohol effect. Initiation of drinking during adolescence, with or without marijuana co-use, disordered normal brain growth trajectories. Factors possibly contributing to abnormal cortical volume trajectories include peak consumption in the past year and family history of alcoholism. (Pfefferbaum A, Kwon D, Brumback T, Thompson WK, Cummins K, Tapert SF, Brown SA, Colrain IM, Baker FC, Prouty D, De Bellis MD, Clark DB, Nagel BJ, Chu W, Park SH, Pohl KM, Sullivan EV. Am J Psychiatry. 2017 Oct 31:appiajp201717040469. doi: 10.1176/appi.ajp.2017.17040469. Epub ahead of print)
Significance: This study utilized a double-blind placebo-controlled human laboratory paradigm to investigate the effects of intravenous (IV) ghrelin administration on alcohol self-administration in heavy-drinking individuals with alcohol dependence. It also investigated the effects of IV ghrelin on reward processing using an fMRI-based task. Results demonstrate that, as compared to placebo, ghrelin increased alcohol self-administration and amygdala activation in the presence of alcohol cues. These data indicate that ghrelin signaling affects alcohol seeking in humans and should be further investigated as a promising target for developing novel medications for alcohol use disorder.
Preclinical evidence suggests that ghrelin, a peptide synthesized by endocrine cells of the stomach and a key component of the gut-brain axis, is involved in alcohol seeking as it modulates both central reward and stress pathways. However, whether and how ghrelin administration may impact alcohol intake in humans is not clear. For, we believe, the first time, this was investigated in the present randomized, crossover, double-blind, placebo-controlled, human laboratory study. Participants were non-treatment-seeking alcohol-dependent heavy-drinking individuals. A 10-min loading dose of intravenous ghrelin/placebo (3 mcg kg-1) followed by a continuous ghrelin/placebo infusion (16.9 ng/kg/min) was administered. During a progressive-ratio alcohol self-administration experiment, participants could press a button to receive intravenous alcohol using the Computerized Alcohol Infusion System. In another experiment, brain functional magnetic resonance imaging was conducted while participants performed a task to gain points for alcohol, food or no reward. Results showed that intravenous ghrelin, compared to placebo, significantly increased the number of alcohol infusions self-administered (percent change: 24.97±10.65, P=0.04, Cohen's d=0.74). Participants were also significantly faster to initiate alcohol self-administration when they received ghrelin, compared to placebo (P=0.03). The relationships between breath alcohol concentration and subjective effects of alcohol were also moderated by ghrelin administration. Neuroimaging data showed that ghrelin increased the alcohol-related signal in the amygdala (P=0.01) and modulated the food-related signal in the medial orbitofrontal cortex (P=0.01) and nucleus accumbens (P=0.08). These data indicate that ghrelin signaling affects alcohol seeking in humans and should be further investigated as a promising target for developing novel medications for alcohol use disorder. (Farokhnia M, Grodin EN, Lee MR, Oot EN, Blackburn AN, Stangl BL, Schwandt ML, Farinelli LA, Momenan R, Ramchandani VA, and Leggio L. Mol Psychiatry. 2017 Nov 14. doi: 10.1038/mp.2017.226. Epub ahead of print)
Rehabilitating the Addicted Brain with Transcranial Magnetic Stimulation
Significance: This review addresses the neurobiological rationale for the potential use of repetitive transcranial magnetic stimulation (rTMS) to treat patients with addictive disorders. Drawing on data from preclinical and clinical studies, the review suggests that changing specific subcortical neural circuits through rTMS of frontal brain regions results in substantial behavioral changes.
This finding suggests that rTMS may be a useful treatment in addition to existing behavioral and pharmacotherapies for addictive disorders.
Substance use disorders (SUDs) are one of the leading causes of morbidity and mortality worldwide. In spite of considerable advances in understanding the neural underpinnings of SUDs, therapeutic options remain limited. Recent studies have highlighted the potential of transcranial magnetic stimulation (TMS) as an innovative, safe and cost-effective treatment for some SUDs. Repetitive TMS (rTMS) influences neural activity in the short and long term by mechanisms involving neuroplasticity both locally, under the stimulating coil, and at the network level, throughout the brain. The long-term neurophysiological changes induced by rTMS have the potential to affect behaviours relating to drug craving, intake and relapse. Here, we review TMS mechanisms and evidence that rTMS is opening new avenues in addiction treatments. (Diana M, Raij T, Melis M, Nummenmaa A, Leggio L, and Bonci A. Nat Rev Neurosci. 2017 Nov; 18(11):685-693. doi: 10.1038/nrn.2017.113. Epub 2017 Sep 29)
Significance: The efficacy of varenicline as a treatment for alcohol use disorder was evaluated in a 16-week clinical trial in 131 alcohol-dependent individuals who also smoked cigarettes. Varenicline significantly reduced heavy drinking in men but not in women. Smoking cessation counseling was not provided, but varenicline resulted in higher smoking abstinence, a finding consistent with the primary indication for varenicline.
Individuals with alcohol use disorder have high rates of cigarette smoking. Varenicline tartrate, an approved treatment for smoking cessation, may reduce both drinking and smoking. To test the efficacy of varenicline with medical management for patients with alcohol use disorder and comorbid smoking seeking alcohol treatment, and to evaluate the secondary effects on smoking abstinence. This phase 2, randomized, double-blind, parallel group, placebo-controlled trial was conducted at 2 outpatient clinics from September 19, 2012, to August 31, 2015. Eligible participants met alcohol-dependence criteria and reported heavy drinking (≥5 drinks for men and ≥4 drinks for women) 2 or more times per week and smoking 2 or more times per week; 131 participants were randomized to either varenicline or placebo stratified by sex and site. All analyses were of the intention-to-treat type. Data analysis was conducted from February 5, 2016, to September 29, 2017. Varenicline tartrate, 1 mg twice daily, and matching placebo pills for 16 weeks. Medical management emphasized medication adherence for 4 weeks followed by support for changing drinking. Of 131 participants, 39 (29.8%) were women and 92 (70.2%) were men, the mean (SD) age was 42.7 (11.7) years, and the race/ethnicity self-identified by most respondents was black (69 [52.7%]). Sixty-four participants were randomized to receive varenicline, and 67 to receive placebo. Mean change in PHDD between varenicline and placebo across sex and site was not significantly different. However, a significant treatment by sex by time interaction for PHDD (F1,106 = 4.66; P = .03) revealed that varenicline compared with placebo resulted in a larger decrease in log-transformed PHDD in men (least square [LS] mean difference in change from baseline, 0.54; 95% CI, -0.09 to 1.18; P = .09; Cohen d = 0.45) but a smaller decrease in women (LS mean difference, -0.69; 95% CI, -1.63 to 0.25; P = .15; Cohen d = -0.53). Thirteen of 45 men (29%) had NHDD taking varenicline compared with 3 of 47 men (6%) taking placebo (Cohen h = 0.64; 95% CI, 0.22-1.03), whereas 1 of 19 women (5%) had NHDD compared with 5 of 20 women (25%) taking placebo (Cohen h = -0.60; 95% CI, -1.21 to 0.04). Taking varenicline, 8 of 64 participants (13%) achieved prolonged smoking abstinence; no one (0 of 67) quit smoking taking placebo (P = .003; Cohen h = 0.72; 95% CI, 0.38-1.07). Varenicline with medical management resulted in decreased heavy drinking among men and increased smoking abstinence in the overall sample. Varenicline could be considered to promote improvements in men with these dual behavioral health risks. ClinicalTrials.gov Identifier: NCT01553136. (O’Malley SS, Zweben A, Fucito LM, Wu R, Piepmeier ME, Ockert DM, Bold KW, Petrakis I, Muvvala S, Jatlow P, and Gueorguieva R. JAMA Psychiatry 2017 Dec 20; doi: 10.1001/jamapsychiatry.2017.3544. Epub ahead of print)
Significance: Cognitive-behavioral approaches have received significant empirical support in the treatment of alcohol and other substance use disorders (SUDs). While a significant amount of evidence has documented the efficacy of CBT for SUDs, little is known about how CBT interventions are disseminated into healthcare settings or how technology may assist in implementation of CBT in these settings. This review provides an overview of and recommendations for avoiding this potential “implementation cliff” and discusses how technology, cognitive science, and neuroscience may provide important clues for the mechanisms that underlie how CBT operates for those with a SUD.
Cognitive–behavioral therapy (CBT) approaches have among the highest level of empirical support for the treatment of drug and alcohol use disorders. As Psychology of Addictive Behaviors marks its 30th anniversary, we review the evolution of CBT for the addictions through the lens of the Stage Model of Behavioral Therapies Development. The large evidence base from Stage II randomized clinical trials indicates a modest effect size with evidence of relatively durable effects, but limited diffusion in clinical practice, as is the case for most empirically validated approaches for mental health and addictive disorders. Technology may provide a means for CBT interventions to circumvent the “implementation cliff” in Stages III–V by offering a flexible, low-cost, standardized means of disseminating CBT in a range of novel settings and populations. Moreover, returning to Stage I to reconnect clinical applications of CBT to recent developments in cognitive science and neuroscience holds great promise for accelerating understanding of mechanisms of action. It is critical that CBT not be considered as a static intervention, but rather one that constantly evolves and is refined through the stage model until the field achieves a maximally powerful intervention that addresses core features of the addictions. (Carroll KM and Kiluk BD. Psychol Addict Behav. 2017 Dec;31(8):847-861. doi: 10.1037/adb0000311. Epub 2017 Aug 31)
Significance: Few studies have targeted alcohol use among people living with HIV/AIDS (PLWHA), possibly due to the prioritization of other challenges (e.g., medication adherence, HIV-related stigma, mental health concerns), limited clinic time, competing life stressors, or other barriers. This meta-analysis evaluated the efficacy of behavioral interventions to reduce alcohol use among PLWHA. Findings showed that these interventions were efficacious in reducing high-risk alcohol, sexual, and nonadherent behaviors that are known to be associated with secondary HIV transmission and poor clinical outcomes. Continued development, testing, and refinement of interventions to reduce alcohol use among PLWHA is needed, as are strategies to integrate alcohol interventions into clinical care.
Alcohol use is often reported among people living with HIV/AIDS (PLWHA) and is associated with increased sexual risk and poor medication adherence. This meta-analysis evaluated the efficacy of behavioral interventions addressing alcohol use among PLWHA. Twenty-one studies (N = 8461 PLWHA) that evaluated an individual-level intervention addressing alcohol use alone or as part of a more comprehensive alcohol/HIV intervention, included a control condition, and were available through December 2016 were included. Independent raters coded study, sample, and intervention content. Weighted mean effect sizes, using random-effects models, were calculated. Results indicate that interventions reduced alcohol consumption, increased condom use, and improved medication adherence relative to controls (d +s = 0.10-0.24). Plasma viral load was also reduced in intervention versus control participants (d + = 0.14, 95% CI = 0.02, 0.26; k = 7). These findings show that behavioral interventions addressing alcohol use can successfully reduce alcohol consumption and also improve HIV-related outcomes among PLWHA. (Scott-Sheldon LAJ, Carey KB, Johnson BT, Carey MP, and MASH Research Team. AIDS Behav. 2017 Nov; 21(Suppl 2):126-143. doi: 10.1007/s10461-017-1886-3)
Significance: Previous studies of alcohol-related emergency department (ED) visits are outdated or examine visits related to acute alcohol use only. This study gives national estimates of ED visits over a nine-year period between 2006 and 2014 related to chronic and acute alcohol use among all ages. Findings indicate a 61% increase in the number of alcohol-related ED visits during the time period assessed, with a 272% increase in costs of these visits. The increase in ED visits was higher among women than men.
BACKGROUND: Acute alcohol consumption and chronic alcohol consumption increase the burden
placed on emergency departments (EDs) by contributing to injury and disease. Whether the prevalence of alcohol-related ED visits in the United States has changed in recent years is unknown. The purpose of this study was to examine trends in ED visits involving acute and chronic alcohol consumption in the United States by age and sex between 2006 and 2014. METHODS: Data from the Nationwide Emergency Department Sample (NEDS), the largest all-payer ED database in the United States involving 945 hospitals in 33 states and Washington, DC, were analyzed to assess changes in prevalence and rates of ED visits involving acute and chronic alcohol consumption by age and sex over time among persons aged ≥12 between 2006 and 2014. RESULTS: Between 2006 and 2014, the number of ED visits involving alcohol consumption increased 61.6%, from 3,080,214 to 4,976,136. The rate increased 47% from 1,223 to 1,802 per 100,000 population and the total cost of such visits increased 272% from $4.1 billion to $15.3 billion. The number of acute alcohol-related ED visits increased 51.5% from 1,801,006 to 2,728,313 and the rate increased 40% from 720.9 to 1,009.6 per 100,000 population. The number chronic alcohol-related visits increased 75.7% from 1,279,208 to 2,247,823 and the rate increased 57.9% from 502.2 to 792.9 per 100,000. The annual percentage change in rates of all alcohol-related ED visits was larger for females than for males (5.3% vs. 4.0%). Other drug involvement increased the likelihood of admission for inpatient treatment. CONCLUSIONS: Alcohol consumption contributed to an increasing number of ED visits in the United States between 2006 and 2014, especially among females. Increased utilization of evidence-based interventions is needed. (White A, Slater ME, Ng G, Hingson R, and Breslow, R. Alcohol Clin Exp Res. 2018 Feb;42(2):352-359. doi: 10.1111/acer.13559. Epub 2018 Jan 2.)
Press and Publications Activities:
Recent News Media Interviews: Dr. Koob continues to speak with a variety of national and international news outlets on timely topics related to NIAAA’s research and its impact on treatment and prevention of alcohol misuse and AUD. Notable interviews since September 2017 include the Associated Press (AP), The Guardian, National Public Radio (NPR), U.S. News & World Report, Time, Vice.com, Inside Higher Ed, The San Diego Union-Tribune, Wired, SiriusXM Doctor Radio, Medscape Medical News, and Science.
Press Releases:
- NIAAA honors Penny S. Mills with Senator Harold Hughes Award (September 14, 2017)
- NIAAA Alcohol Treatment Navigator points the way to quality treatment (October 3, 2017)
- George F. Koob, Ph.D., elected to the National Academy of Medicine (October 16, 2017)
- Dr. Kenneth J. Sher to deliver 22nd Annual Mark Keller Honorary Lecture at the National Institutes of Health (November 27, 2017)
- NIH study shows steep increase in rate of alcohol-related ER visits (January 12, 2018)
Satellite Media Tour: On January 9, 2018, NIAAA conducted a satellite media tour (SMT) with Dr. Koob on the topic of looking back at the holidays and recognizing signs of an alcohol-related problem, as well as promoting the new NIAAA Alcohol Treatment Navigator as a resource. Dr. Koob completed 20 live and recorded interviews with television and radio stations around the country, including stations from Los Angeles, California; Baltimore, Maryland, Philadelphia, Pennsylvania; Milwaukee, Wisconsin; Tucson, Arizona; Detroit, Michigan; and Memphis, Tennessee. In addition, USA Radio Network will be distributing an interview nationwide and California Life HD-TV will air an interview which will reach viewers throughout the state of California. “Talk with Audrey,” a syndicated TV and radio talk show hosted by Audrey Adams, will be airing an interview on selected stations around the country. In addition to the SMT interviews conducted on January 9, Dr. Koob participated in a live listener call-in interview with SiriusXM Doctor Radio’s “Healthy Aging” program on January 8, 2018, and an in-studio interview on January 29, 2018, with KUSI-TV News, San Diego. According to preliminary estimates, the combined reach of the satellite media tour thus far is estimated to be 8.45 million individuals. This estimate should increase as final numbers are provided in the coming weeks.
Publication Statistics: Since September 2017, NIAAA has filled orders for approximately 65,900 copies of print publications. As of November 27, 2017, there were 30,286 GovDelivery/Granicus subscribers to Alcohol Research: Current Reviews; 21,575 to the NIAAA Spectrum; and 21,278 to receive general information.
Social Media Highlights:  The NIAAA Twitter account (@NIAAAnews) currently has more than 19,600 followers and averages about 100,0
The NIAAA Twitter account (@NIAAAnews) currently has more than 19,600 followers and averages about 100,0 00 impressions (number of times users saw the tweet on Twitter) per month. NIAAA has held two Twitter chats since the last Council meeting – one in October 2017 with the launch of the Alcohol Treatment Navigator and another in December 2017 on women’s health and alcohol. Dr. Ducharme served as the chat expert for the #TreatmentNavigator chat, co-hosted with ASAM. The chat had an estimated reach of 1.63 million impressions (the number of times any tweets from the chat could have been seen). The Twitter chat on women and alcohol was held December 14, 2017, in partnership with the National Council on Alcoholism and Drug Dependence (NCADD). Dr. Deidra Roach served as chat expert for an event with an estimated reach of 5.3 million impressions and 1.48 million accounts reached. Top chat contributors include NCADD, U.S. Department of Health and Human Services, womenshealth.gov, the LEAF Council on Alcoholism and Addictions, National Organization on Fetal Alcohol Syndrome, NIDA, @USAlcoholPolicy, and NAADAC (The Association for Addiction Professionals). On January 16, 2018, NIAAA participated in a trans-NIH townhall #NIHHealthy2018, about adopting healthy habits for the new year. The chat hashtag had such broad reach, it trended nationally for more than three hours.
00 impressions (number of times users saw the tweet on Twitter) per month. NIAAA has held two Twitter chats since the last Council meeting – one in October 2017 with the launch of the Alcohol Treatment Navigator and another in December 2017 on women’s health and alcohol. Dr. Ducharme served as the chat expert for the #TreatmentNavigator chat, co-hosted with ASAM. The chat had an estimated reach of 1.63 million impressions (the number of times any tweets from the chat could have been seen). The Twitter chat on women and alcohol was held December 14, 2017, in partnership with the National Council on Alcoholism and Drug Dependence (NCADD). Dr. Deidra Roach served as chat expert for an event with an estimated reach of 5.3 million impressions and 1.48 million accounts reached. Top chat contributors include NCADD, U.S. Department of Health and Human Services, womenshealth.gov, the LEAF Council on Alcoholism and Addictions, National Organization on Fetal Alcohol Syndrome, NIDA, @USAlcoholPolicy, and NAADAC (The Association for Addiction Professionals). On January 16, 2018, NIAAA participated in a trans-NIH townhall #NIHHealthy2018, about adopting healthy habits for the new year. The chat hashtag had such broad reach, it trended nationally for more than three hours.
On November 17, 2017, NIAAA participated in the Institute’s first Facebook Live event with the Addiction Policy Forum. Drs. Lori Ducharme and Patricia Powell served as panelists for an hour-long discussion of the Alcohol Treatment Navigator livestreamed on Facebook.
Partnerships, Outreach & Public Liaison Activities:
 Winter Holiday Outreach
Winter Holiday Outreach
NIAAA disseminated its fact sheet, “The Truth About Holiday Spirits: Celebrate Safely This Holiday Season” via PR Newswire on December 12 and December 20, 2017, resulting in links from 255 outlets and a potential audience of 70 million. Outlets included Yahoo!, local newspaper websites, numerous local television outlets nationwide, and blogs focusing on parenting or food and wine/spirits. The fact sheet image was posted on Cision’s Times Square billboard 10 times during December. NIAAA also tweeted seasonal messages throughout December, including PSAs on cocktail content, blood alcohol content, and the risks underestimating the effects of alcohol. For the first time as part its seasonal outreach, NIAAA issued a media availability that also resulted in a number of high-profile interviews.
NIAAA Alcohol Treatment Navigator Launch and Promotion
In October 2017, NIAAA launched its new NIAAA Alcohol Treatment Navigator website, with a comprehensive, multi-faceted package of promotional activities.
News Outreach: News coverage resulting from these activities was extensive, and appeared nationwide in print, online, and in broadcast media. NIAAA worked with Lauran Neergaard of the Associated Press for a story titled “Trying to Get Sober? NIH Offers Tool to Find Good Care,” which was timed with the Navigator’s launch and included interviews with Drs. George F. Koob and Lori Ducharme. This AP story was carried by 393 outlets around with country, with a potential audience of more than 516 million people and an earned publicity value of $380,000. Outlets included The New York Times, U.S. News & World Report, The Washington Post, the Los Angeles Times, and the Chicago Tribune. An additional AP-TV story was aired by 12 broadcast outlets, including WPIX New York, KTBS Shreveport, WXIN Indianapolis, and WBAL Baltimore, with a potential audience of 230,000 people. NIAAA further disseminated a multimedia news release via PR Newswire, which had 255 links and a potential audience of 117 million people. In addition, NIAAA communications pitched the story to targeted media outlets, writers, and bloggers, resulting in additional pickup including two notable NPR opportunities–Allison Aubrey’s piece “Is Alcohol a Problem? Online Tool Helps Assess Risk and Find Help,” which aired January 8, 2018, on Morning Edition and an hour-long discussion on NPR’s 1A, featuring Drs. Lori Ducharme and Aaron White. The NPR coverage resulted in more than 100 mentions in the media, with a total estimated reach of 85.6 million people. High-profile media exposure such as this continues to increase national coverage and traffic to the website.
Social Media: Robust social media promotion of the Alcohol Treatment Navigator with Twitter graphics and videos generated 4.8 million total potential impressions during its launch week. Partner organizations such as AASLD, ASAM, Guard Your Health, National Association for Children of Alcoholics, and the National Library of Medicine’s MedlinePlus helped amplify promotion by tweeting messages about the Navigator as well. Soon after the launch, NIAAA conducted a webcast demonstration of the website to 182 interested community members and partnered with the Addiction Policy Forum in November 2017 for a live run-through and panel discussion. Dr. Ducharme led a Twitter chat about the Navigator in partnership with ASAM, which generated 1.6 million impressions. Ongoing digital promotion and social media outreach is planned for 2018. 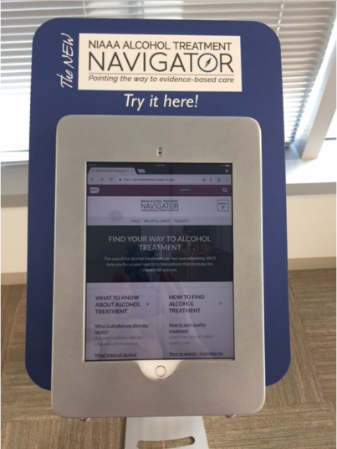
Web Activities: Rotating graphics and messages about the Treatment Navigator have been placed in the carousel on the NIAAA homepage, and the website has been enhanced to improve visibility. Search engine optimization and other efforts are underway to maximize traffic to Navigator website.
Professional Meetings and Conferences: NIAAA has created an interactive kiosk that allows attendees at conferences and professional events to explore the Navigator website. The Navigator will be promoted at future meetings and will be centerpiece of NIAAA’s exhibit at the 2018 NBC4 health fair, which will be held at the Walter E. Washington Convention Center in Washington, D.C. Advertisements will be inserted in meeting information packages and pitching sessions/presentations at national meetings and professional conferences.
Liaison Groups: Dozens of liaison groups published information about the Navigator through social media, newsletters, and other platforms.
Amplifying Our Outreach: NIAAA reached out to multiple platforms to amplify promotional messages about the Navigator via news stories, blog posts, and social media. A single story or posting can reach millions of broadcast viewers and/or social media followers, resulting in supplemental news pieces that further promote NIAAA’s messages. One such example is an editorial written by Dr. Keith Humphreys, Professor at Stanford University, titled “Have a drinking problem? Here’s a tool for finding effective treatment” published in The Washington Post in January 2018.
Select Partnership Updates
The National Association of State Alcohol & Drug Abuse Directors featured a presentation on the Treatment Navigator from Dr. Ducharme during their All States Public Policy Call on November 17, 2017. On February 6, 2018, NIAAA presented at Community Anti-Drug Coalitions of America (CADCA’s) 2018 National Leadership Forum. Dr. Koob presented on NIAAA research priorities; Dr. Ducharme presented on the Navigator; and Dr. Ralph Hingson presented “The Stories Behind the Statistics: Interventions that Work to Prevent Underage Drinking.”
National Drug and Alcohol Facts Week (NDAFW): NIAAA partnered with NIDA on NDAFW, a week of events geared towards educating young people and parents about the dangers of drugs and alcohol, which took place during the week of January 22-28, 2018.
New Director’s Blog
The NIAAA Director’s blog launched in October 2017. In his first post, Dr. Koob discussed the NIAAA Alcohol Treatment Navigator.
Web Activities
NIAAA has expanded communications activities with the NIH Clinical Research Trials and You website. Recently, the website linked to an article on NIAAA’s website about results of an NIAAA intramural trial published in the American Journal of Psychiatry.

