Cross-Cutting Research Programs
Cross-cutting research programs are NIAAA-managed research portfolios that include topics spanning multiple research goals outlined in this strategic plan. These programs complement the Cross-Cutting Research Themes and Supporting the Mission sections of this strategic plan.
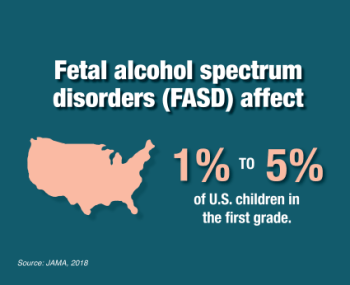
Fetal Alcohol Spectrum Disorders
Fetal alcohol spectrum disorders (FASD) represent the broad range of neurodevelopmental impairments and other physical effects that result from prenatal exposure to alcohol. NIAAA supports a robust FASD research program to advance study of the causes, mechanisms, diagnosis, prevention, and treatment of FASD.
Research to reduce stigma around prenatal alcohol exposure, to increase education and awareness of FASD, and to develop culturally appropriate prevention strategies are important components of FASD prevention. Basic research on the biological mechanisms that underlie prenatal alcohol exposure and contribute to FASD can lead to the identification of diagnostic biomarkers as well as potential treatment targets, paving the way for earlier diagnosis and treatment. NIAAA is also facilitating efforts to reach consensus on a single research classification system for FASD to harmonize research efforts across the globe and accelerate scientific progress
Objective 1: Advance the Prevention of Prenatal Alcohol Exposure
Preventing and reducing alcohol use during pregnancy is essential to preventing prenatal alcohol exposure and related consequences, including FASD. Studies have shown that alcohol screening, brief intervention, and referral to treatment (SBIRT) approaches are an effective tool for addressing alcohol and other substance use in primary and prenatal care settings.
NIAAA encourages research and other activities to prevent and reduce prenatal alcohol exposure and the prevalence of FASD—for example:
- Designing and evaluating cost-effective models to help women at high risk of having a child with FASD (i.e., who misuse alcohol, have alcohol use disorder (AUD), or already have another child with FASD) to reduce or abstain from drinking during pregnancy and, consequently, reduce the incidence of FASD
- Developing culturally informed interventions to prevent alcohol-exposed pregnancies
- Improving implementation and enhancing scalability of effective preventive interventions (e.g., alcohol SBIRT) for alcohol misuse and its negative consequences in women
- Identifying the causes of FASD-related stigma and exploring strategies to reduce it in order to improve prevention efforts
- Promoting collaboration with federal and nonfederal organizations to raise public awareness about FASD and advance implementation of prevention interventions in various clinical and nonclinical settings
Objective 2: Improve Early Identification and Treatment Interventions for Fetal Alcohol Spectrum Disorders
Improved diagnostic techniques for FASD could enable more accurate diagnosis, expand access to assessment for FASD, allow for earlier intervention, and likely reduce costs and overall burden of FASD across the life span. Early identification holds promise for better outcomes, but limited availability of FASD diagnostic services remains a barrier to care.
NIAAA encourages research to enhance FASD screening, diagnosis, and treatment—for example:
- Improving implementation of existing evidence-based FASD diagnostic approaches across the life span as well as early intervention and care for individuals with FASD across a range of populations and settings, such as for children and parents in the child welfare system and individuals in the juvenile justice system
- Developing novel technologies and methods to facilitate earlier identification of children affected by prenatal alcohol exposure, as early as the fetal and newborn periods
- Assessing combinations of evidence-based therapeutic approaches for individuals with FASD
- Understanding and addressing health disparities concerning prenatal alcohol exposure in different populations
- Developing and evaluating novel prenatal and postnatal therapeutic approaches, medications, and dietary supplements to combat prenatal alcohol exposure and FASD
- Pursuing various interventions to mitigate the neurocognitive and behavioral deficits associated with FASD across the life span
Objective 3: Identify Mechanisms, Diagnostic Biomarkers, and Potential Treatment Targets for Fetal Alcohol Spectrum Disorders
Alcohol can disrupt prenatal development through a variety of mechanisms. Understanding the biological effects of prenatal alcohol exposure that emerge across the life span, from prenatal development to adulthood, can inform preventive and therapeutic strategies to mitigate the consequences of prenatal alcohol exposure.
NIAAA encourages research to advance foundational knowledge of the mechanisms mediating FASD—for example:
- Identifying and characterizing the biological mechanisms underlying the harmful effects of prenatal alcohol exposure across the life span, including health consequences that persist or emerge in adults with FASD
- Further defining periods of susceptibility to alcohol exposure (e.g., periconception, specific months or trimester, entire pregnancy, or time points during postnatal development)
- Elucidating the potential paternal contribution to the etiology of FASD
- Refining and advancing biomarkers of prenatal alcohol exposure
- Defining the long-term health impacts of prenatal alcohol exposure in later adulthood
Alcohol and HIV
Alcohol is an important contributor to the HIV pandemic. In the United States, many people with HIV engage in alcohol misuse or have AUD. Alcohol can affect behaviors that increase the likelihood of acquiring or transmitting HIV to others. Alcohol may also speed HIV progression in people living with the disease, influence their engagement and retention in HIV treatment, and increase their susceptibility to organ damage and coinfections. These effects may shift across the life span, particularly as people living with HIV enter midlife and older adulthood.
In coordination with the NIH Office of AIDS Research and the NIH Strategic Plan for HIV and HIV-Related Research, NIAAA continues to advance basic, translational, and clinical research to improve health outcomes among people living with HIV, including women and underserved populations who experience health disparities. NIAAA will enhance collaboration with partners within and outside NIH to translate and disseminate research findings to maximize the public health impact of NIAAA-supported HIV research, and to strengthen the research and workforce capacity to sustain alcohol-HIV research.
Objective 1: Understand the Biological and Behavioral Mechanisms of Alcohol Misuse and HIV
The mechanisms through which alcohol misuse interacts with HIV to increase morbidity and mortality are not well understood. While HIV can be treated effectively with antiretroviral medications, alcohol misuse contributes to or exacerbates adverse medication interactions, chronic inflammation, liver and other organ injury, cardiovascular and neurological problems, and other pathologies.
Several biological or behavioral phenotypes of HIV and alcohol have been identified that may have markedly different disease courses, biological underpinnings, and treatment responses. Collaborative, multidisciplinary research will be key to better understanding the interactions between alcohol misuse and HIV.
NIAAA encourages research to better understand the relationship between alcohol misuse and HIV to inform the development of effective interventions—for example:
- Determining how alcohol misuse confers a biological risk for HIV infection
- Determining how current and past alcohol misuse in the context of HIV infection and the use of antiretroviral medications affect HIV disease progression and the development of organ and tissue injury (e.g., gut, liver, lung, and brain)
- Improving the understanding of the biological, clinical, and socio-behavioral aspects of aging through the lens of HIV infection and alcohol misuse
Objective 2: Prevent Alcohol Misuse and Treat Alcohol Use Disorder Among People Living With HIV or at High Risk of Acquiring HIV
As noted above, alcohol misuse contributes to poor health outcomes among people living with HIV and reduces the effectiveness of strategies designed to prevent new HIV infections. For example, the use of pre-exposure prophylaxis (PrEP) is highly effective in preventing HIV among those at high risk. However, alcohol misuse may reduce a person’s likelihood of following PrEP medication regimens.
Alcohol misuse may also affect an individual’s adherence to antiretroviral therapy and contribute to HIV transmission. Evidence-based approaches, such as brief interventions, contingency management, risk and harm reduction interventions, and stepped care approaches, have been demonstrated to prevent and reduce alcohol misuse among people living with HIV. Stepped care approaches that integrate treatment for alcohol misuse and HIV have also been shown to improve HIV-related outcomes. Strategies to identify and address alcohol misuse among people with HIV or at high risk for HIV can contribute to improved health and a reduced incidence of HIV.
NIAAA encourages alcohol-related research to prevent and reduce HIV infection, progression, and transmission—for example:
- Enhancing routine alcohol SBIRT to reduce HIV transmission and disease progression
- Developing strategies that address alcohol-related barriers to effective use of PrEP, especially among women and other populations with historically low usage rates
- Developing novel interventions and enhancing implementation of existing evidence-based prevention and treatment interventions that address both alcohol misuse and HIV
- Expanding access to and options for AUD treatment for people living with HIV
Objective 3: Address Alcohol-Related Comorbidities Among People Living With HIV
Many comorbidities, coinfections, and medical complications are associated with chronic alcohol misuse and HIV disease progression. These factors combine with the natural processes of aging to increase frailty and present challenges for medical management. Addressing comorbid medical complications is critical for improving quality of life and longevity.
NIAAA encourages research to address alcohol-related comorbidity among individuals with HIV—for example:
- Promoting the integration of care for HIV, alcohol misuse or AUD, and co-occurring health conditions and medical complications in different settings
- Developing a comprehensive model for alcohol misuse or AUD and disease outcomes among older adults with HIV, including expanded biomarker assays
- Evaluating the efficacy and effectiveness of interventions for reducing alcohol misuse in improving co-occurring pain, stress, and other mental health concerns among people living with HIV

