Objective 1: Enhance Treatment Options for Alcohol Use Disorder and Related Conditions
Currently, there are three medications for AUD approved by the FDA, and they are effective and important treatment aids. Still, given the multiple biological processes that contribute to AUD, new medications are needed to provide a broader spectrum of treatment options.
Pharmacotherapy, especially when combined with behavioral interventions, is an effective, evidence-based component of AUD treatment. NIAAA encourages research to develop a larger number of pharmaceutical treatments for AUD, because people deserve to choose from a range of evidence-based treatment options that can be tailored to their individual needs. In addition, improving the precision of diagnosis could improve patient outcomes. Because AUD is a complex, highly heterogeneous condition, some individuals may, for example, respond best to a medication that helps with craving and relieves impulsivity, whereas others may respond best to a medication that reverses the negative emotional state of withdrawal or protracted withdrawal symptoms.
ALD, a spectrum of liver diseases caused by alcohol misuse, is the most common alcohol-related cause of death. There are no FDA-approved medications for ALD, and current standard medical treatment, such as steroids, may have significant side effects. Through the NIAAA-supported Alcohol-associated Hepatitis Network, researchers can use and contribute to ALD research and gain insights into the causes and treatments of ALD and integrated treatment of ALD and AUD. Development of drugs that act on multiple molecular targets to reverse and prevent progression of liver damage and to reduce alcohol intake can open new opportunities. Research may identify similar strategies for other alcohol-associated organ damage.
AUD also frequently co-occurs with sleep, pain, and mental health disorders, such as anxiety disorders. Medications to address these co-occurring conditions, in coordination with AUD, could vastly improve health outcomes.
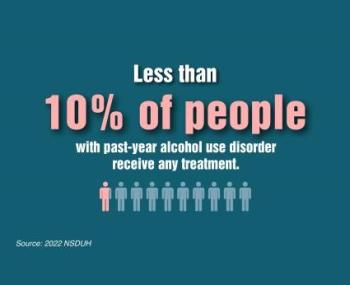
Developing effective pharmacotherapies to address AUD, ALD, and other co-occurring conditions and increasing their uptake continue to be major priorities for NIAAA. NIAAA encourages research to support these priorities, for example:
- Harnessing computational and data science approaches to identify and evaluate biological, cognitive, and behavioral markers, endophenotypes, and clinical characteristics that can be used to predict an individual’s response to specific treatments or treatment combinations
- Developing biomarker and biomarker signatures to serve as surrogate endpoints for intervention clinical trials and to improve clinical management of alcohol-associated health conditions
- Validating alternative outcome measures for alcohol pharmacotherapy trials that will be accepted by the FDA for phase II and III trials (i.e., a two-level reduction in the World Health Organization drinking risk levels)
- Developing new or repurposing existing medications to treat AUD, ALD, and other alcohol-associated organ dysfunction such as alcohol-associated pancreatitis and acute respiratory distress syndrome
- Using pharmacoepidemiological approaches to identify potential medication targets to either co-opt existing medications for use in alcohol-related conditions or facilitating the development of new medications, if necessary
- Leveraging high-throughput multi-omics, artificial intelligence (AI), machine learning, and other statistical approaches to identify molecular signatures and other potential targets linked to pharmacotherapy for AUD
- Developing high-throughput screening platforms for discovery of medications to treat AUD
- Exploring new human laboratory paradigms that will help predict efficacy in clinical trials for AUD/ALD medications development
- Assessing the impact of concurrent use of medications for AUD and other co-occurring disorders on, for example, drug interactions and altered drug pharmacokinetics
- Exploring strategies to design innovative clinical trials to study one or more specific phenotype-targeted therapies in the context of co-occurring disorders in AUD patients