The Cycle of Alcohol Addiction
Alcohol addiction is a chronic relapsing disorder associated with compulsive alcohol drinking, the loss of control over intake, and the emergence of a negative emotional state when alcohol is no longer available. Alcohol use disorder (AUD) is a condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It is a spectrum disorder and can be mild, moderate, or severe and encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, or the colloquial term, alcoholism. Alcohol addiction refers to the moderate to severe end of the AUD spectrum.
How Does Addiction Develop in the Brain?
Alcohol, like other drugs, has a powerful effect on the brain, producing pleasurable feelings and blunting negative feelings. These feelings can motivate some people to drink alcohol again and again, despite possible risks to their health and well-being. For example, research shows that over time, drinking to cope with stress—while it may provide temporary relief from emotional discomfort—tends to enhance negative emotional states between bouts of alcohol consumption. These changes can motivate further drinking and cause an individual to become stuck in an unhealthy cycle of alcohol consumption.1,2
As individuals continue to drink alcohol over time, progressive changes may occur in the structure and function of their brains. These changes can compromise brain function and drive the transition from controlled, occasional use to chronic misuse, which can be difficult to control. The changes can endure long after a person stops consuming alcohol, and can contribute to relapse in drinking.
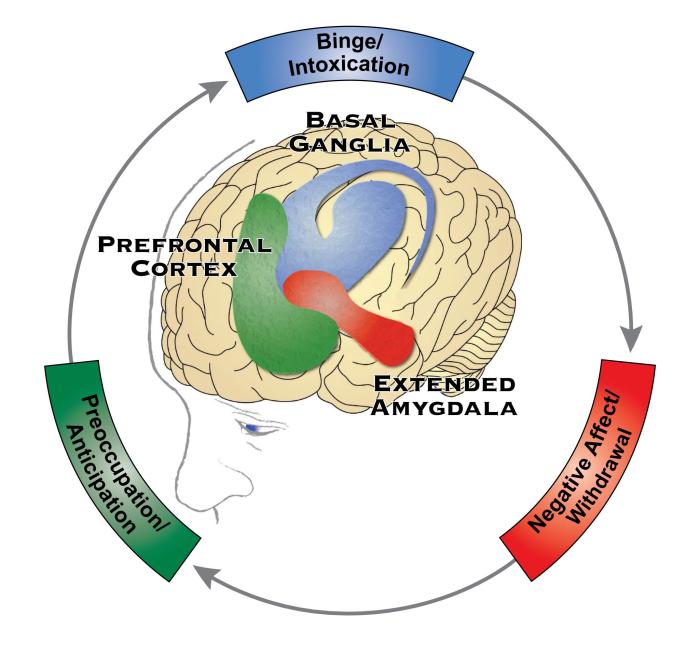
Stages of the Addiction Cycle
Addiction can be framed as a repeating cycle, with three stages. Each stage is linked to and feeds on the others. These stages primarily involve three domains: incentive salience, negative emotional states, and executive function. The domains are reflected in three key regions of the brain: the basal ganglia, the extended amygdala, and the prefrontal cortex, respectively. A person may go through this three-stage cycle over the course of weeks or months, or progress through it several times in a day.3,4,5 Note also that a person can enter the cycle of addiction at any one of the following stages:
1. Binge/Intoxication Stage: reward, incentive salience, and pathological habits
- During this stage, a person experiences the rewarding effects of alcohol, such as euphoria, the reduction of anxiety, and the easing of social interactions.
- Repeated activation of the basal ganglia’s reward system reinforces alcohol drinking behavior, increasing the likelihood of repeated consumption. The basal ganglia play an important role in motivation as well as in the formation of habits and other routine behaviors.
- This repeated activation of the basal ganglia also ultimately triggers changes in the way a person responds to stimuli associated with drinking alcohol, such as specific people, places, or alcohol-associated cues such as certain glassware or images or descriptions of drinking. Over time, these stimuli can trigger powerful urges to drink alcohol.
- Repeated alcohol consumption also results in changes in the basal ganglia that lead to habit formation, ultimately contributing to compulsive use.
2. Negative Affect/Withdrawal Stage: reward deficits and stress surfeit
- When a person who is addicted to alcohol stops drinking, they experience withdrawal symptoms—or symptoms that are opposite to the positive effects of alcohol that are experienced when drinking it. These symptoms can be physical (sleep disturbances, pain, feelings of illness) and emotional (dysphoria, irritability, anxiety, and emotional pain).
- The negative feelings associated with alcohol withdrawal are thought to come from two sources. First, a diminished activation in the reward systems—or a reward deficit—of the basal ganglia makes it difficult for people to experience the pleasures of everyday living. Second, an increased activation of the brain’s stress systems—or a stress surfeit—in the extended amygdala contributes to anxiety, irritability, and unease.
- At this stage, the person no longer drinks alcohol for the pleasurable effects (“high”), but rather to escape the “low” feelings to which chronic alcohol misuse has contributed.
3. Preoccupation/Anticipation Stage: craving, impulsivity, and executive function
- This is the stage at which an individual seeks alcohol again after a period of abstinence. A person becomes preoccupied with alcohol and how to get more of it, and looks forward to the next time he or she will consume it.
- The prefrontal cortex—an area of the brain responsible for executive function, including the ability to organize thoughts and activities, prioritize tasks, manage time, and make decisions—is compromised in people experiencing alcohol addiction. As a result, this area of the brain plays a key role in this stage.
Hyperkatifeia
Hyperkatifeia is a word that can be used to describe the negative emotional state associated with drug withdrawal. This overactive negative emotional state is hypothesized to drive the consumption of alcohol to find relief from this emotional state, and it may be caused by profound changes in the brain reward and stress systems.
Why Should We Be Concerned About AUD and Alcohol Addiction?
Alcohol consumption is linked to many health and social consequences, including interference with personal relationships, heart and liver diseases, cancers, motor vehicle collisions and other accidents, alcohol overdose, violence, homicide, and suicide. If a person has AUD, particularly if it is moderate to severe and involves alcohol addiction, they are more likely to regularly consume alcohol in levels associated with these effects on health.
Young people are especially at risk for AUD. Using alcohol during adolescence (from preteens to mid-20s) may affect brain development, making it more likely that they will be diagnosed with AUD later in life. However, most people with AUD—no matter their age or the severity of their alcohol problems—can benefit from treatment with behavioral health therapies, medications, or both.
For more information about how alcohol affects the brain, please visit Alcohol and the Brain, and for more information about available evidence-based treatments for AUD, please visit the NIAAA Alcohol Treatment Navigator.
1 Armeli, S.; Sullivan, T.P.; and Tennen, H. (2015). Drinking to cope motivation as a prospective predictor of negative affect. Journal of Studies on Alcohol and Drugs 76(4):578–584, 2015. PMID: 26098033
2 Wardell, J.D.; Kempe, T., Rapinda, K.K.; et al. Drinking to cope during COVID-19 pandemic: The role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcoholism, Clinical and Experimental Research 44(10):2073–2083, 2020. PMID: 32870516
3 S. Department of Health and Human Services. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf. Accessed December 8, 2021.
4 Koob, G.F.; and Volkow, N.D. Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry 3(8):760–773, 2016. PMID: 27475769
5 Koob, G.F., Powell, P., and White, A. Addiction as a coping response: Hyperkatifeia, deaths of despair, and COVID-19. The American Journal of Psychiatry 177(11):1031–1037, 2020. PMID: 33135468

